Locked Into Place
Much has been learned about exertional rhabdomyolysis (tying-up) in recent years, but unfortunately some of that knowledge has been troubling. For example, at least one newly recognized cause of tying-up in foals has, in identified cases, always
Much has been learned about exertional rhabdomyolysis (tying-up) in recent years, but unfortunately some of that knowledge has been troubling. For example, at least one newly recognized cause of tying-up in foals has, in identified cases, always been fatal. This syndrome, known as glycogen branching enzyme deficiency (GBED), is an inherited malady for which there is no known cure. For years, researchers and horse owners thought that tying-up in all horses had a common cause. However, research has shown that there are multiple causes and that successful treatment protocols can vary from horse to horse.
There is still much to learn about tying-up. Genetic tests are needed to determine which horses carry the genes that make them susceptible to this affliction. Stephanie J. Valberg, DVM, PhD, of the University of Minnesota, has been a leading researcher on tying-up. Before arriving at the University of Minnesota in 1994, Valberg was involved in studies and research at the Swedish University of Agricultural Sciences in Uppsala, Sweden, where she obtained her PhD, and later at the University of California, Davis.
Perhaps one of the reasons that researchers and horse owners were convinced for years that there was a single cause for tying-up is that no matter what triggers the disorder, the clinical signs are similar. Afflicted horses suffer varying degrees of pain, muscle cramping, and stiffness in the rear quarters. With some horses it might involve stiffness when walking, and in others the pain might be so severe that they writhe on the ground, similar to a horse with colic
Create a free account with TheHorse.com to view this content.
TheHorse.com is home to thousands of free articles about horse health care. In order to access some of our exclusive free content, you must be signed into TheHorse.com.
Start your free account today!
Already have an account?
and continue reading.
Written by:
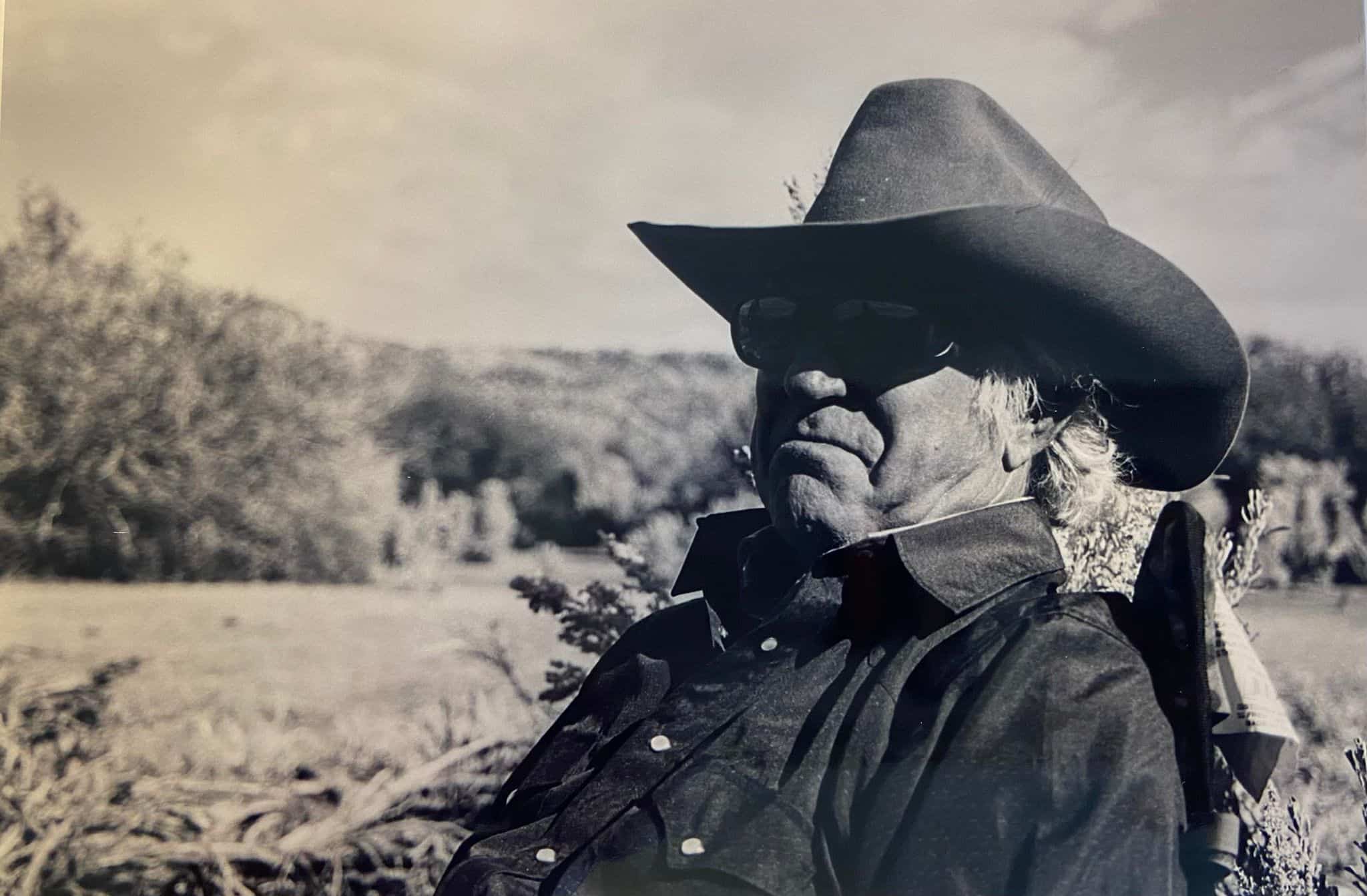
Les Sellnow
Related Articles
Stay on top of the most recent Horse Health news with















