Obesity and Cushing’s Disease
- Topics: Article
Cushing's disease has been around for a long time in people, horses, and other animals. For years, theories and information concerning the affliction all centered on one source for the problem–tumors of the pituitary gland, which is located at the base of the brain. In the case of horses, it was generally felt that benign tumors in the intermediate lobe of the horse's pituitary gland resulted in an inappropriate secretion of hormones, which brought on Cushing's disease. Nowadays, the correct term is pituitary pars intermedia dysfunction (PPID), since it has been discovered that degeneration of the hypothalamic dopaminergic neurons (those in the hypothalamus using dopamine as their neurotransmitter) is the primary cause.

For years, theories and information concerning Cushing's disease all centered on one source for the problem–inappropriate secretion of hormones caused by tumors of the pituitary gland, which is located at the base of the brain. Nowadays, the correct term is pituitary pars intermedia dysfunction (PPID) since it has been discovered that degeneration of the hypothalamic dopaminergic neurons (those in the hypothalamus using dopamine as their neurotransmitter) is the primary cause.
There is an affliction that has some of the same characteristics as Cushing's, yet is different. At the same time, there is speculation that this syndrome, termed metabolic syndrome and previously called peripheral Cushing's syndrome, could be a factor in horses which develop Cushing's disease
Create a free account with TheHorse.com to view this content.
TheHorse.com is home to thousands of free articles about horse health care. In order to access some of our exclusive free content, you must be signed into TheHorse.com.
Start your free account today!
Already have an account?
and continue reading.
Written by:
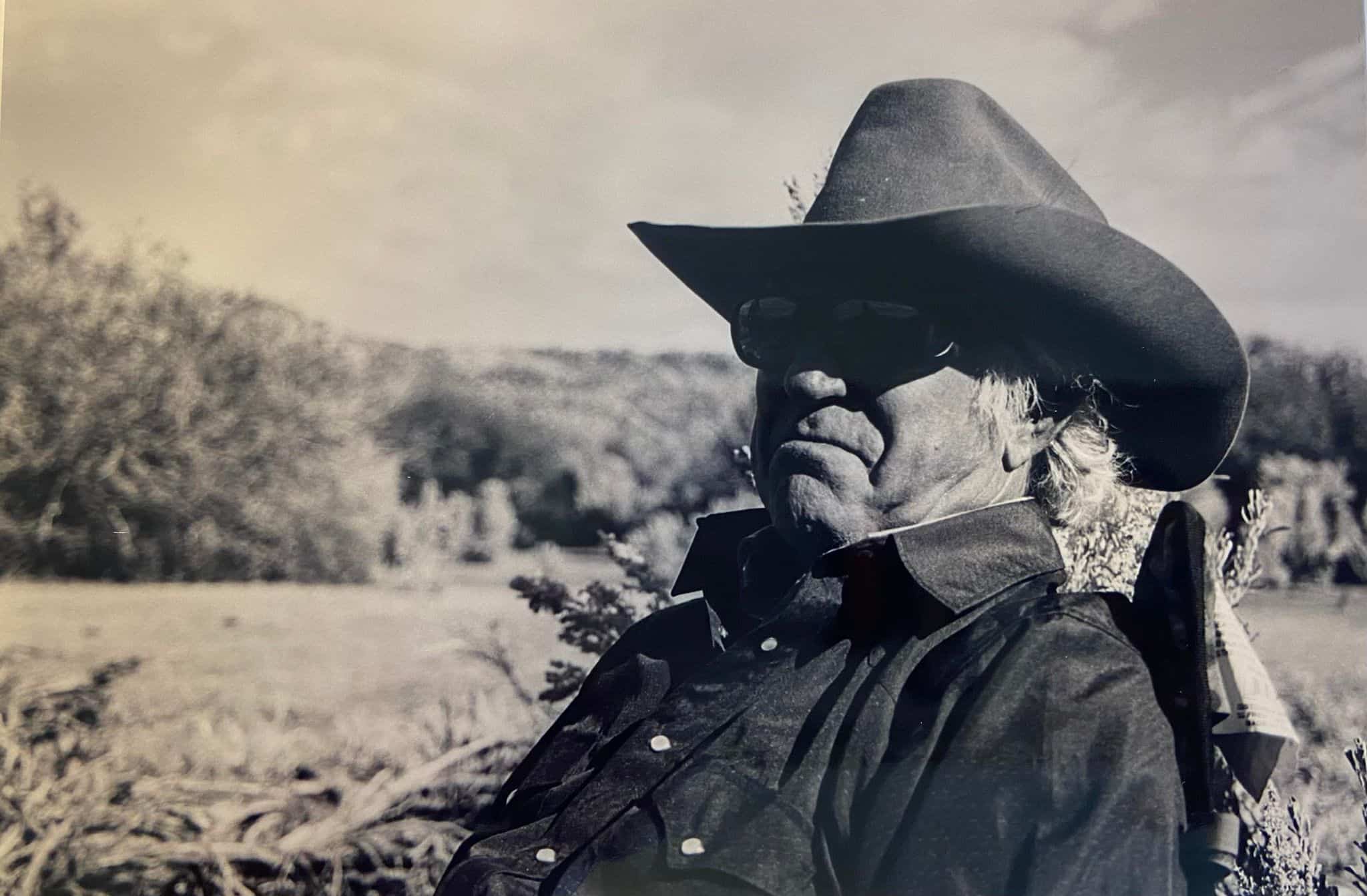
Les Sellnow
Related Articles
Stay on top of the most recent Horse Health news with















