Encephalomyelitis
The initials are innocuous enough–EEE, WEE, VEE–but the diseases they stand for can be deadly to both equines and humans. They are, in order, Eastern Equine Encephalomyelitis (EEE), Western Equine Encephalomyelitis (WEE), and Venezuelan Equine
Share
ADVERTISEMENT
Create a free account with TheHorse.com to view this content.
TheHorse.com is home to thousands of free articles about horse health care. In order to access some of our exclusive free content, you must be signed into TheHorse.com.
Start your free account today!
Already have an account?
and continue reading.
Share
Written by:
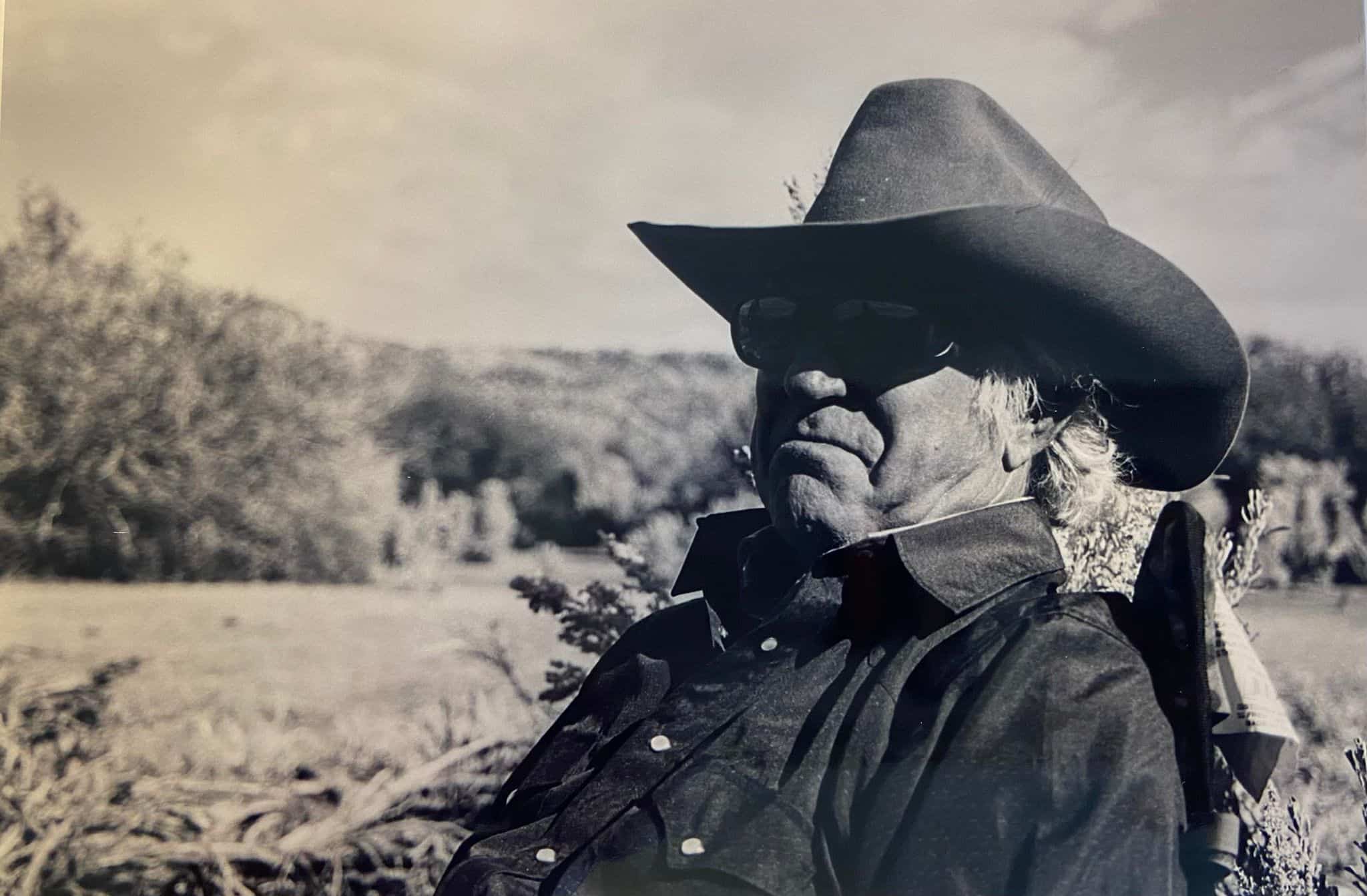
Les Sellnow
Les Sellnow was a prolific freelance writer based near Riverton, Wyoming. He specialized in articles on equine research, and operated a ranch where he raised horses and livestock. He authored several fiction and nonfiction books, including Understanding Equine Lameness and Understanding The Young Horse. He died in 2023.
Related Articles
Stay on top of the most recent Horse Health news with












