Retina and Optic Nerve Disease in Horses
Editor’s Note: This article was revised by the author to reflect new and updated information in November 2017.
In the last article of the 12-part series on the equine eye, we focus on diseases of the retina and optic nerve
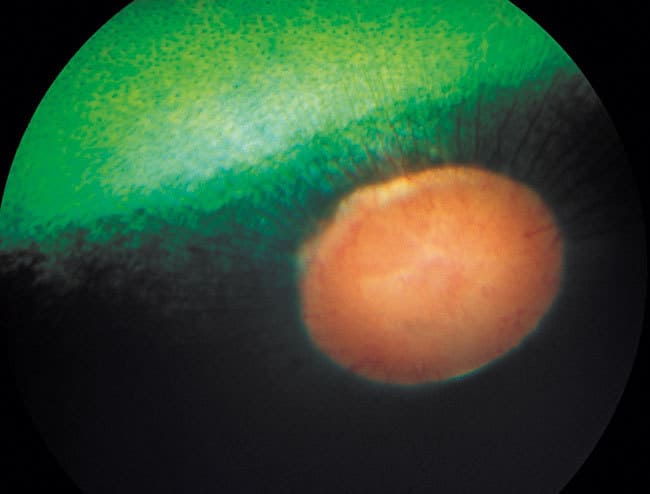
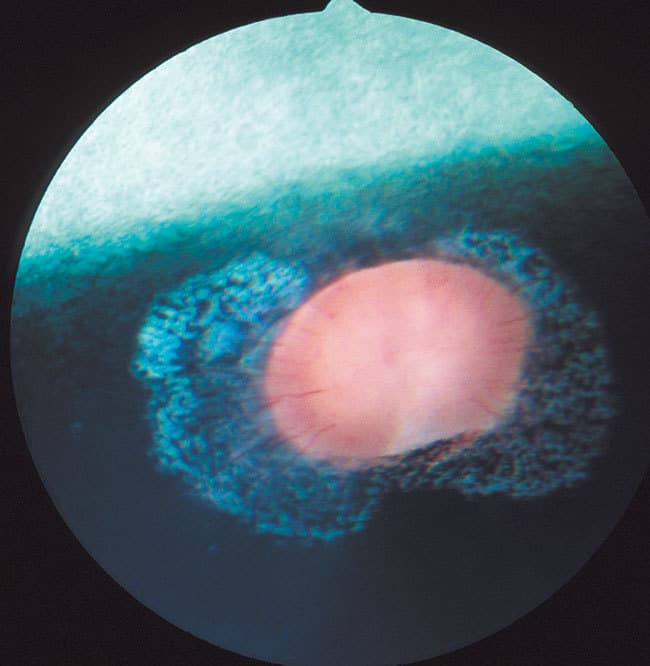
The retina is one of the most metabolically active tissues in the body. It consists of 10 layers of cells and nerve fibers. Nine layers compose the sensory retina, with a final layer, the retinal pigment epithelium (RPE), present next to the choroids (the primary blood supply to the horse retina). Light passing through the cornea, anterior chamber, lens, and vitreous is absorbed and organized by retinal cells, which then transform the light into electrical signals that pass along the optic nerve fibers to the brain. A reflective tissue called the tapetum in the upper choroid improves night vision. The retina, retinal blood vessels, tapetum, and optic disc (the front of the optic nerve) can be seen with special instruments called ophthalmoscopes. Diseases of the retina and optic nerve are respectively termed retinopathies and optic neuropathies.
Create a free account with TheHorse.com to view this content.
TheHorse.com is home to thousands of free articles about horse health care. In order to access some of our exclusive free content, you must be signed into TheHorse.com.
Start your free account today!
Already have an account?
and continue reading.
Written by:
Dennis E. Brooks, DVM, PhD, Dipl. ACVO
Related Articles
Stay on top of the most recent Horse Health news with















